

October 23, 2024
I have a question for you guys to answer. But for that, I need you to step yourself into the shoes of a healthcare business owner. Here is what I want you to answer: “What do you want to achieve through your business?” Let me make a wild guess about your response.
Some of you might have said that their sole purpose is to deliver high-quality patient care, while others might have been honest about their end goal and acknowledged generating revenue. For those whose response was patient care, I am sure you don’t want to overlook the importance of financial sustainability. This is where healthcare revenue cycle management comes into play.
Today, I will break down everything about revenue cycle management in healthcare, which is a crucial process for improving financial performance.
Revenue cycle management (RCM) is a process that helps healthcare businesses track and manage their billing operations and collect revenue for the services they provide. The revenue cycle process doesn’t start with billing; it begins with patient registration and insurance verification and covers everything in between to end at payment collection.
RCM helps organizations gain financial stability by generating accurate claims and expediting payment collection processes. Moreover, there is a significant surge in the global revenue cycle management market, which is $148.84 billion in 2024 and will reach $361.86 billion by 2032. This expansion is enough to highlight the importance of revenue cycle management.

You can understand the importance of the revenue cycle management process by the fact that it can make or break a healthcare business. I am going to make the complete revenue cycle process simple for you. Here is an easy explanation of the RCM process or stages:
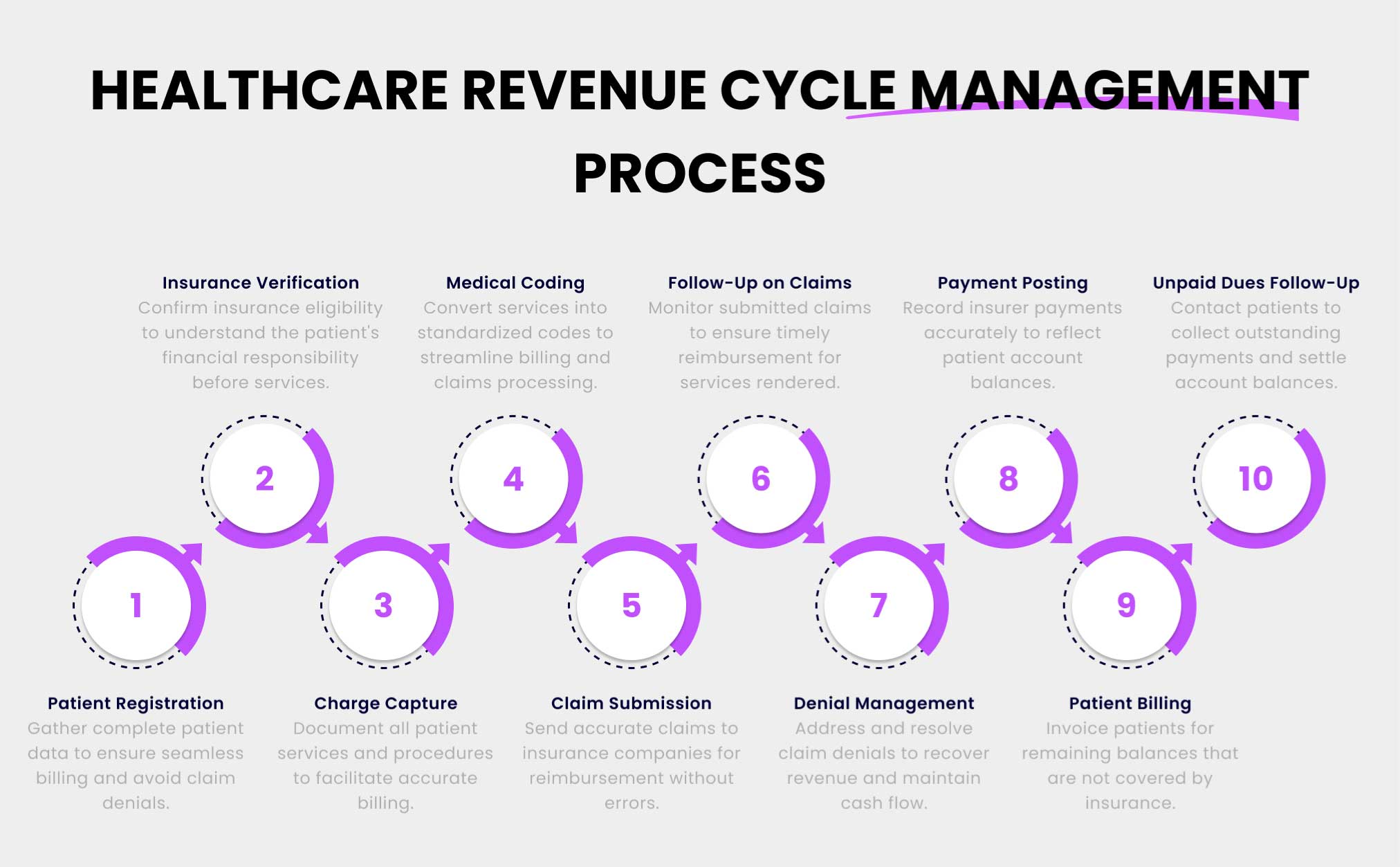
The first stage of RCM is to collect complete patient information. It can be the patient’s demographic, contact information, insurance information, medical history, etc. This process is essential for both the new and the returning patients. It helps to keep the data up-to-date and avoid any claim denials.
The next step in the medical revenue cycle management process is to verify the patient’s insurance eligibility. Here, it is necessary to know that this must be done before providing services to patients. It is crucial for both the providers and patients in order to know the patient’s financial responsibility and what insurance covers.
After doing the initial steps and providing the necessary services to a patient, the next stage is charge capture. It is a stage where the complete patient journey from the time of appointment to the services and procedures performed are recorded. These records are stored in the electronic medical record systems to make them accessible to every authorized person.
After everything is recorded, it is time to translate the services or procedures into standardized medical codes, i.e., ICD-10, HCPCS, and CPT codes. These codes are used instead of mentioning the complete services to reduce errors in billing processes and speed up claim processing. These codes help calculate the reimbursement amounts that healthcare providers will receive.
Most small and medium healthcare businesses, due to lack of resources and time, outsource the claims handling process to top medical billing companies. It is a process of generating claims and then submitting them to the insurance companies for reimbursement. This step requires keen attention, as a slight mistake can lead to claim denial and finance leakage.
Once the claims are submitted, the next step in the revenue cycle process is to track the status of the claims. If the healthcare provider isn’t reimbursed for the provided services within 20 days, it is necessary to follow up to get every dollar you spend on delivering patient care.
In case your claim is denied, healthcare providers must understand the reasons for denials, address those issues, and resubmit the claims to recover lost revenue and improve cash flow. Either the provider will get the payment from the insurer, or else the claim will be considered a loss and written off.
After getting the payment from the insurer, the next step is to post payment in the patient’s account. It is a very crucial stage of the revenue cycle management in medical billing. This step is about matching the payment with the bill and recording any due balance correctly.
The next step in the healthcare revenue cycle management is to bill patients for the remaining balance that the insurance didn’t cover. It can be co-pay, deductibles, or payment for non-covered services. It helps healthcare providers to be compensated fully for the provided services.
The last phase of revenue cycle management in healthcare is to follow-up patients on unpaid dues. Healthcare providers must contact them using the patient contact details they provide during registration, i.e., by email or by phone, to collect outstanding payments.
Revenue cycle management is one of the most crucial processes that holds significant importance for healthcare providers. It is because of the numerous benefits that RCM offers that no one can deny. The investment in healthcare RCM will help you reap the following benefits:
Handing over your revenue cycle management processes to a reliable medical billing company or implementing RCM software allows providers to reduce operational costs. They can do so by automating routine administrative tasks, like billing, coding, claims generation and submission, etc. It helps to reduce the burden and stress on your team.
RCM frees up resources and enables them to prioritize patient care to achieve better patient outcomes. Moreover, it helps healthcare providers cut labor costs and minimize costly errors. What’s more, RCM solutions provide financial reports that enable organizations to identify areas where costs can be further reduced.
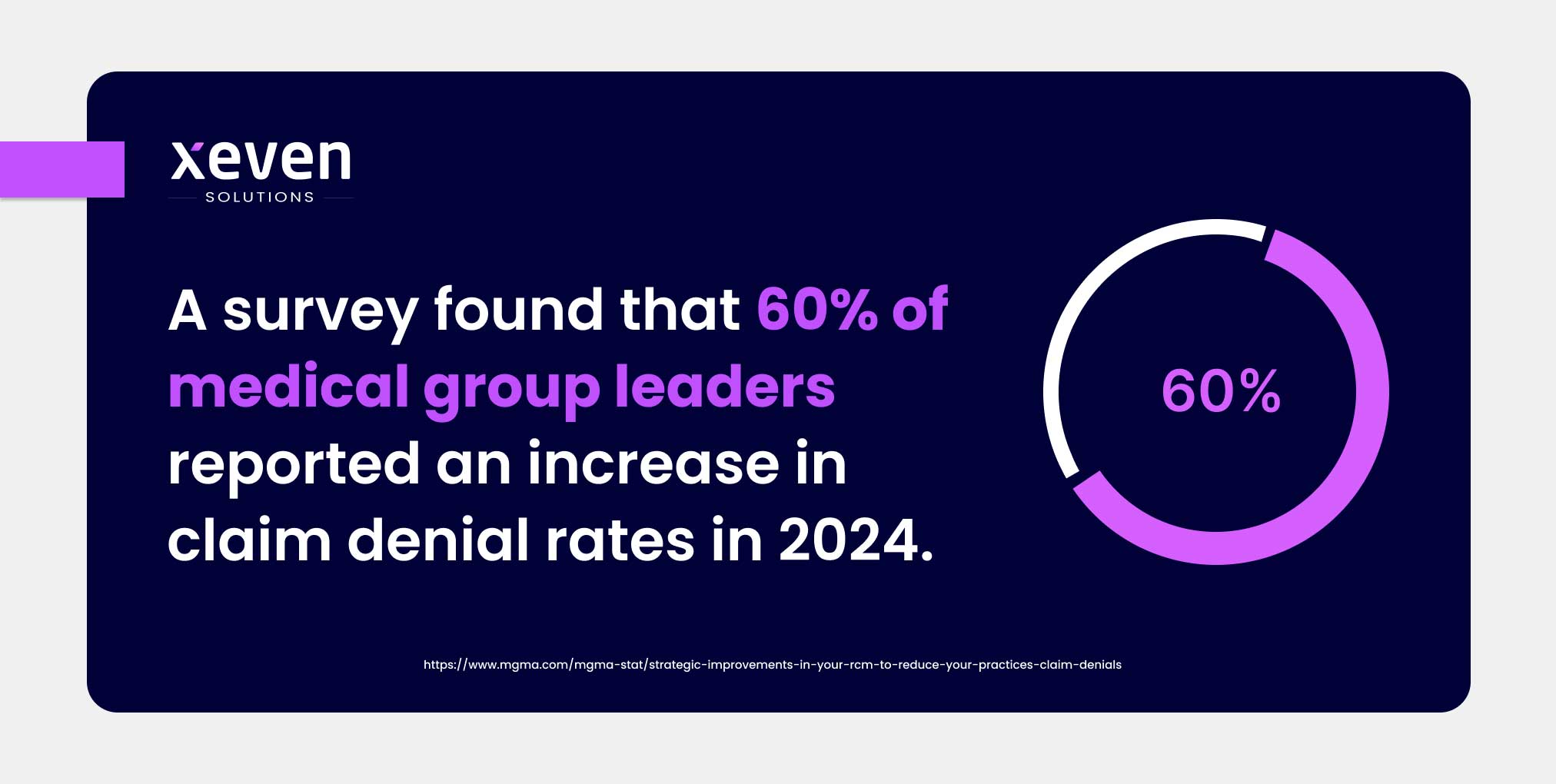
A survey found that 60% of medical group leaders reported an increase in claim denial rates in 2024. To my surprise, 46% of respondents reveal missing or inaccurate information to be one of the biggest reasons behind claim denials.
Medical revenue cycle management helps healthcare providers reduce claim denials by submitting accurate claims. The claim denial can occur due to coding or billing errors, duplicate claims, insurance eligibility, etc. Reliable RCM systems or service providers focus on all these aspects and ensure that all claims are accurately processed. It helps healthcare providers to avoid financial leakages and get reimbursed quickly without any delays.
We all know that in today’s world, everyone—be it a customer or a patient—wants the best experience. That’s exactly what revenue cycle management in medical billing offers. It helps to make billing and scheduling processes convenient for patients, thus improving their experience.
There is transparency and no errors during billing, which reduces confusion and helps to improve provider-patient relationships. Moreover, verifying insurance eligibility before the appointment allows patients to understand how much money they have to pay and what expenses their insurance company will cover.
RCM enables healthcare providers to not only improve cash flow but also increase revenue. Healthcare providers can eliminate billing and coding errors and can verify insurance eligibility to generate accurate claims. Accurate claims submission means no denying and faster reimbursements for the services rendered.
Healthcare providers spend $19.7 billion each year on resolving denial disputes with insurance companies. This means that by avoiding claims denials, healthcare providers can avoid huge financial losses and gain peace of mind.
If any healthcare provider thinks that they can deliver exceptional care without optimizing your processes, think again. It is crucial for organizations to optimize their medical revenue cycle process to stop financial losses and gain stability. Here are some best practices in revenue cycle management to follow:
The efficiency of revenue cycle management (RCM) can be increased significantly by making sure that healthcare providers collect comprehensive patient information. It may include patient demographics, contact information, insurance details, etc. It helps to prevent one of the biggest reasons for claims denials, which is incomplete or incorrect details. By doing so, healthcare providers can accelerate the reimbursement process.
One of the revenue cycle management best practices is to verify patient insurance information before providing services. In the verification process, providers must confirm what the insurance will cover and what the patient is responsible for paying. It helps to reduce claim denials and understand insurance payment responsibilities upfront.
Organizations must optimize the claim management process to speed up the reimbursement process. It involves everything from claim generation to denial management. Prioritizing follow-up on submitted claims and resubmission of denied claims is also necessary to get paid for the services provided.
Keeping a keen eye on the complete lifecycle of claims helps you understand the loopholes to avoid delays in payment collection. However, it is understandable that healthcare providers have to focus on patient care and don’t have enough time. So, the best thing they can do is to consider outsourcing or automation for better claim management.
Another best practice to follow in improving revenue cycle management in medical billing is to build trust with patients. Healthcare providers can achieve this by informing patients about their financial responsibilities and insurance coverage. It helps to reduce payment collection issues, enhance patient satisfaction, and earn their loyalty.
Continuously monitor key KPIs in revenue cycle management to measure the health of revenue cycle management. Providers can consider multiple factors, including days in accounts receivable, clean claim rates, and denial rates. These factors help providers to identify areas for improvement and make necessary adjustments.
If you aren’t willing to outsource medical billing revenue cycle management, then it is a best practice to educate and train your staff. Healthcare providers can provide training on coding regulations and claim management processes to make sure that their staff has the right skills. It also helps them to improve staff productivity and reduce errors while handling healthcare revenue cycle management.
Modern technologies are more than just a necessity these days for better medical revenue cycle management. Numerous healthcare software solutions, including electronic health records (EHRs) and billing systems, are available to help healthcare providers enhance revenue cycle efficiency. Using these solutions simplifies processes, reduces manual errors, and provides valuable data insights for improving the revenue cycle process.
Most smaller businesses don’t have enough resources to handle revenue cycle management in healthcare and provide high-quality patient care. SMEs don’t need to overburden their staff and help them prioritize what they do best. I recommend SMEs save resources for more strategic tasks and outsource RCM medical billing processes to a reliable third-party vendor. Outsourcing offers numerous benefits, including access to experts, saving costs, and efficient RCM.
Xeven Solutions has been one of the top revenue cycle management companies in the business for over a decade. We have helped businesses from around the globe to improve cash flow and expedite payment collection by generating accurate claims.
Our well-versed medical billing experts identify loopholes in your revenue cycle process, like inaccurate coding and managing denied claims, to help you stop revenue leakage and maximize reimbursements. Get in touch with our experts to speed up claim submission and reduce errors in billing to gain financial stability.